Sickle Cell Disease care is now receiving global attention, thanks to the World Health Organization’s newly released guidelines. These global guidelines aim to improve early diagnosis, ensure access to essential medicines like hydroxyurea, and provide lifelong support for people living with this inherited blood disorder. With better care systems, millions of lives—especially in Africa, India, and low-income countries—can be saved or improved.
What is Sickle Cell Disease and Why Care Matters
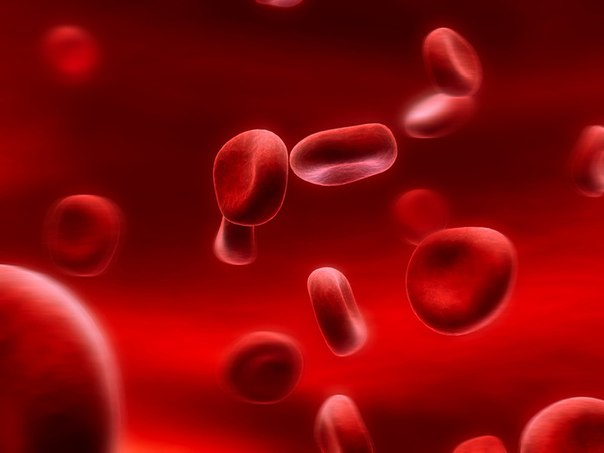
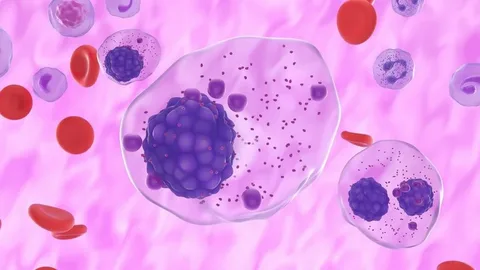
Sickle Cell Disease, or SCD, is a genetic blood disorder. That means a person is born with it and inherits it from their parents.
In this disease, red blood cells, which are normally round and soft, become hard and shaped like a sickle or crescent. These abnormal cells can block blood flow and break apart too soon. This leads to problems such as:
- Severe pain (known as a sickle cell crisis)
- Frequent infections
- Anemia
- Organ damage
- Stroke
- Shortened life span if untreated
Why Sickle Cell Disease Care is a Global Priority
Sickle Cell Disease is a global public health concern. It mostly affects people in:
- Sub-Saharan Africa
- India
- The Middle East
- South America
- Some Mediterranean countries
More than 300,000 babies are born with the disease each year. Without proper diagnosis and treatment, many children die before they reach the age of five. Those who survive often face a lifetime of pain, frequent hospital visits, and loss of school and work opportunities.
WHO’s Role in Strengthening Sickle Cell Disease Care
The World Health Organization, or WHO, is an international health body that works to improve global health. It helps countries prevent and treat diseases and promotes better healthcare systems.
In June 2024, WHO released its first-ever global guidelines for managing Sickle Cell Disease. These guidelines are important because they offer clear steps for how countries can improve diagnosis, treatment, and lifelong care for people with SCD. They aim to reduce suffering, improve survival rates, and ensure access to affordable care.
WHO Guidelines for Improving Sickle Cell Disease Care
The WHO guidelines provide a full plan for how to take care of people with SCD. They cover everything from early testing to lifelong support.
Early Screening and Diagnosis in Sickle Cell Disease Care
- All newborn babies should be tested for SCD
- Early diagnosis helps start treatment before serious problems begin
- Countries should include SCD testing in standard health checkups for infants
Preventive Medicines and Vaccines for Sickle Cell Disease Care
- Children with SCD have weaker immune systems
- WHO recommends giving penicillin from age two months to five years
- In areas with malaria, children should also receive malaria prevention
- Routine vaccines should be given to prevent pneumonia, meningitis, and flu
Using Hydroxyurea to Improve Sickle Cell Disease Care
- Hydroxyurea is a medicine that helps reduce the number of sickle cell crises
- It also lowers the need for blood transfusions and improves quality of life
- WHO recommends using hydroxyurea even for children under age five
- It is safe, affordable, and should be made widely available
Safe Blood Transfusions as Part of Sickle Cell Disease Care
- Some patients with SCD need regular blood transfusions
- This is especially important for children at risk of strokes or severe anemia
- Safe and clean blood should always be available
- Patients should be monitored to avoid iron overload from repeated transfusions
Pain Management in Effective Sickle Cell Disease Care
- Pain is a common and serious symptom of SCD
- Health workers should be trained to recognize and treat pain properly
- WHO encourages the use of pain-relief medicine and hydration during crises
- Patients should be treated with dignity and respect during painful episodes
Educating Families for Better Sickle Cell Disease Care
- Education helps families manage the disease better
- Parents should know how to give medicines and when to take their child to the hospital
- Awareness about diet, hydration, and hygiene is also important
Building Lifelong Systems for Sickle Cell Disease Care
- SCD is a lifelong condition
- People with SCD need regular doctor visits, lab tests, and access to specialists
- WHO recommends that countries build sickle cell clinics and include SCD care in national health plans
Global Impact of WHO Guidelines on Sickle Cell Disease Care
The new WHO guidelines are expected to:
- Reduce child deaths from SCD
- Lower the number of hospital admissions
- Make treatment affordable and easier to access
- Help children attend school and adults go to work
- Support national health systems in caring for SCD patients
- Provide equal treatment for rich and poor families
These changes will improve the lives of millions of people and help fight health inequality.
Sickle Cell Disease Care in India and Other Affected Regions
In India, SCD is especially common among tribal populations in states such as:
- Chhattisgarh
- Odisha
- Gujarat
- Maharashtra
- Madhya Pradesh
The Government of India launched the National Sickle Cell Anemia Elimination Mission in 2023. It aims to:
- Provide free testing and treatment
- Distribute hydroxyurea
- Increase public awareness
- Reduce SCD-related deaths by 2047
WHO’s new guidelines will help strengthen this mission by offering global standards and support.
Community Role in Strengthening Sickle Cell Disease Care
Everyone has a part to play in the fight against SCD. Here are some ways people can help:
- Parents should get their babies tested early
- Schools can offer support for students with SCD, including rest time and flexible schedules
- Local communities can hold health awareness events
- Youth groups can spread information through posters and talks
- Social media can be used to share simple health messages
Final Thoughts on Sickle Cell Disease Care
The WHO Guidelines for Sickle Cell Disease Care are an important step toward better health for millions of people. With clear instructions for early testing, treatment, and care, these guidelines can save lives and reduce suffering.
If followed properly by health systems, governments, and families, these guidelines will help more children live longer, healthier lives. They bring hope to those who have long lived in pain and fear.
conclusion:
Sickle Cell Disease is serious, but it can be managed with the right care.
Thanks to the new WHO guidelines, children and adults around the world now have a better chance to live long, healthy lives.
With early diagnosis, proper treatment, and education, we can reduce the pain and suffering caused by SCD and bring hope to millions.
Frequently Asked Questions (FAQ)
About Global Guidelines for Sickle Cell Disease Care:
Q1. What is Sickle Cell Disease?
Answer:
Sickle Cell Disease (SCD) is a genetic blood disorder where red blood cells become hard and sickle-shaped instead of soft and round. These sickle cells can block blood flow and cause pain, infections, and organ damage.
Q2. What is meant by ‘Sickle Cell Disease care’?
Answer:
Sickle Cell Disease care means the regular medical support and treatment needed to help people with SCD live healthier lives. It includes early diagnosis, vaccines, medicines like hydroxyurea, pain management, blood transfusions, and lifelong medical follow-up.
Q3. Why did WHO release guidelines for Sickle Cell Disease care?
Answer:
WHO released the global guidelines to help countries provide better care for people with SCD, especially in places where health services are limited. These guidelines give doctors and governments a clear plan to improve testing, treatment, and support for patients.
Q4. What are some key parts of the WHO guidelines?
Answer:
The WHO guidelines recommend:
- Testing newborns early
- Giving preventive medicines and vaccines
- Using hydroxyurea to reduce pain and hospital visits
- Safe blood transfusions
- Teaching families how to manage SCD
- Building clinics for lifelong care
Q5. What is hydroxyurea and why is it important?
Answer:
Hydroxyurea is a low-cost medicine that helps reduce painful sickle cell crises and lowers the need for blood transfusions. WHO now recommends it even for young children because it’s safe and effective.
Q6. Can children with Sickle Cell Disease go to school and live normally?
Answer:
Yes. With proper care, children with SCD can attend school, play, and live active lives. They might need extra rest or medicines, but they can grow up like other children if they get regular medical support.
Q7. How does early testing help in Sickle Cell Disease care?
Answer:
Early testing helps doctors find out if a baby has SCD before symptoms start. This means treatment can begin early, which can prevent serious problems and save lives.
Q8. Is Sickle Cell Disease curable?
Answer:
There is no simple cure for most people with SCD, but it can be managed. Some bone marrow transplants can cure SCD, but they are not widely available. Most people live longer, healthier lives with regular care.
Q9. Which countries are most affected by Sickle Cell Disease?
Answer:
SCD is most common in parts of Africa, India, the Middle East, South America, and some Mediterranean countries. In India, it mostly affects tribal communities in states like Odisha, Chhattisgarh, Gujarat, and Maharashtra.
Q10. What can families and schools do to support SCD care?
Answer:
- Parents should ensure their children get tested and follow up on medicines
- Schools can allow rest breaks and support children with health needs
- Communities can spread awareness and help families access health services